Table of Content
This includes staff failures to provide CPR, prevent falls, monitor lab results, or report changes in a patient’s condition to physicians. Long before the coronavirus devastated nursing homes, inadequate staffing in for-profit Texas facilities endangered residents, leading to injuries and deaths. Health officials say that as community spread has taken hold, it will soon find its way into nursing homes, which was the case in Texas. Throughout the summer, COVID-19 cases among young adults rapidly rose, leading to the spread of the disease to individuals in long-term care facilities. The Paradigm at First Colony Nursing Home has the eighth-highest number of deaths among nursing homes in the state, tied with three other nursing homes, according to data from state health officials. Officials from the nursing home declined to comment on the timeframe during which the deaths occurred.
Texas provides outbreak totals for resident cases and number of facilities with a case. Texas defines an outbreak as a facility with 1 or more cases in a facility. All Texas data is self-reported by the facility to the Texas Health and Human Services Commission .
Nursing Home Wrongful Death Verdicts
In May, she and her husband had planned a large family celebration for the couple’s 50th wedding anniversary at their favorite place along the river north of Uvalde, but they canceled it because of the pandemic. She remembers a man who was in hospice care and stopped eating when his wife couldn’t visit him every day after the lockdowns began. When the pandemic hit, the couple was close to making a difficult decision to move Lynda into long-term care so she wouldn’t be home alone while Ray was working on the ranch.
The CDC’s recentlyupdated COVID-19 guidance, which is more relaxed, may also contribute to more cases. He would allegedly dress as a maintenance worker or health care aid to get into the homes and kill his victims — whose deaths largely went uninvestigated at the time because they were assumed to have been natural causes due to their ages, People magazine said. Meanwhile, at Texas nursing homes, deaths spiked a second time, with a high of 410 in one week in early January. The holidays brought a fresh round of challenges as state and federal officials told nursing home operators that residents must be allowed to leave and go visit family over Thanksgiving and Christmas. That proportion began to decline as the pandemic became more deadly for people outside of nursing homes.
Share this article:
Mountain View, Rosalie’s facility, decreased its registered nurse staffing ratio by 46 percent the year after it was acquired by Creative Solutions. The facility’s corresponding CMS rating dropped from two stars to one in 2019. Creative Solutions operated with, on average, one registered nurse for every 98 residents in 2019. Mountain View Health & Rehabilitation was acquired in February 2018 by Creative Solutions in Healthcare, a company that owns and operates 64 facilities in Texas and is the state’s second-largest nursing home owner. The Center for Disease Control and Prevention states that due to the congregate nature and the type of residents they take care of , COVID-19 poses a greater risk to nursing home populations. The CDC has developed core practices that these facilities should implement to protect their residents better.
The state health agency launched an investigation into the outbreak at Mountain View and four other Creative Solutions nursing homes in El Paso. State officials said on Thursday that investigations into all of the facilities except Mountain View have been concluded, but they had not provided findings of those investigations to the Observer by Monday. While 68% of Texas facilities reported they had not tested residents since the previous week’s CMS report, 87% of Texas nursing homes indicated they could test all residents within the next week. For context, Texas ranked 47 out of 50 states, tied with Nevada for having one of the lowest percentage of nursing homes able to test all residents within seven days. So far, there have been over 18,000 coronavirus infections among residents across Texas nursing homes; of those, more than 2,000 have died, according to state data.
Facility notes
SB 826, by creating a new Article 49.24, Code of Criminal Procedure, mandates that notification of such a person's death must be made to the OAG within 24 hours of the person's death. Furthermore, it mandates that the facility prepare and submit to the office of the Attorney General, a report containing all facts relevant to the individual's death within 72 hours of the death. Procedures are in place to have affected facilities report the required information by fax or email. Only a small portion of the state’s nursing homes met that criteria at the time. That’s also when the first COVID-19 case showed up at Focused Care at Corpus Christi. There would be 18 more infections and four virus-related deaths among its residents by the end of September, according to state data.

But she avoided catching the virus, even as the nation endured its highest-ever spike in deaths and hospitalizations. Throughout autumn, deaths across the state and the nation began to drop, and nursing homes in Texas saw the same decline. After a few days in an assisted-living facility, Langford moved into Amistad in August. Within a couple of months, the Corpus Christi area became a hot spot, grabbing national headlines when a 6-week-old infant died from the virus and again when nearly a quarter of all tests citywide came back positive for the virus. Within a month, the death toll in Texas nursing homes reached nearly 500.
to 20-year-olds can now carry handguns in Texas
The facilities were already required to report that data to state and local health officials. The state has not disclosed the number of deaths by county in nursing homes and assisted living centers. To curb the spread, Lee said, the state needs to increase transparency and release names of facilities with outbreaks, not just data on infections and deaths, as well as mandate testing of all residents and staff when there is a confirmed case in a facility.
In many instances, nursing homes are not taking the necessary steps to ensure the safety of their residents. New data released by the state health agency provides a glimpse into the infections, deaths, and recoveries at Texas nursing homes. Statewide, 88% of nursing facilities reported they have tested staff and personnel that have shown new signs or symptoms. The overall number of coronavirus-related deaths also saw a significant increase statewide last week, with 33 percent more deaths reported last week than the week prior. Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $15,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states.
The virus is reaching some of the state’s older, more vulnerable residents. Texas’ health system has been underfunded, understaffed, and unprepared for years. “They’re not going to change their staffing for that; that is nothing,” said Tosh, the abuse lawyer. “That is the cost of doing business in Texas.” And since bringing these cases to trial is often so expensive, he said, even the maximum award can be consumed by legal and expert fees. “They have them laying in their own waste because don’t come by enough because they’re understaffed.

In 2019, 74-year-old Lynda took a spill in their home out in the country and broke her arm and shoulder. The pain medication made her dizzy, and even after she stopped taking the meds, her falls happened more frequently. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply. You could be tempted to take heart that the number of cases among long-term care patients has not increased as much as cases for the general population in US hot spots. But considering how much more adverse their outcomes are likely to be, that is actually little solace. And now, according to a new data analysis from the Kaiser Family Foundation, it seems those fears are being realized.
He is dedicated to fighting for justice, and welcomes the opportunity to help you. I know the answer to how much a nursing home wrongful death settlement is because I researched it and listed out the results for you above, which you should read to figure out the value of your case, but the average is between $600,000 and $800,000. Average settlements for nursing home wrongful death cases are not always this high, but in some cases, the situation warrants it.
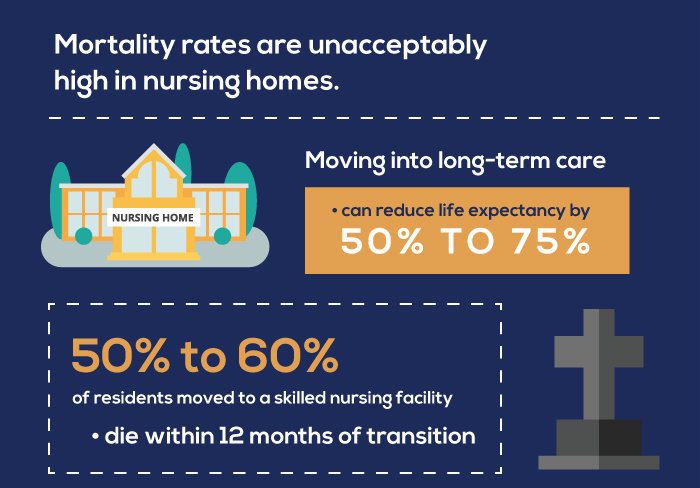
One gives providers more Medicaid money to hire more workers, which provided an estimated $91.5 million to 962 nursing facilities in fiscal year 2020. Another program boosts Medicaid payments to facilities that improve on quality metrics, with funding dedicated to improving recruitment and retention of staffing and increasing the number of daily registered nurse hours in facilities. More than 800 facilities received $66 million in fiscal year 2020 from this component. As of September 27, 2020, there were around 125 COVID-19 deaths per 1,000 residents in nursing homes in Massachusetts.

No comments:
Post a Comment